Can you sleep in the end – At the end of life, the ability to sleep peacefully and comfortably becomes paramount. Delving into the intricacies of sleep patterns during this delicate time, this article explores the physiological, environmental, medical, and psychological factors that influence sleep quality in end-of-life patients.
By gaining a deeper understanding of these factors, we can create a more supportive and restful environment for those facing the end of their journey.
As we navigate the complex landscape of end-of-life care, it is essential to recognize the importance of sleep and its profound impact on overall well-being. By shedding light on the challenges and potential solutions surrounding sleep disturbances, this article aims to empower caregivers and loved ones with the knowledge and tools they need to provide compassionate and holistic care.
Sleep Patterns and the End of Life
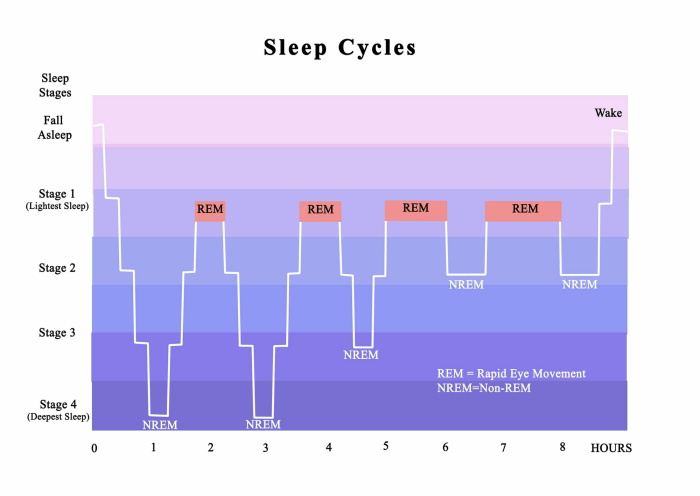
Sleep patterns undergo significant changes towards the end of life. As the body’s systems begin to decline, sleep becomes more fragmented and less restorative. This can lead to a decrease in both the quality and duration of sleep. Common sleep disorders among end-of-life patients include insomnia, sleep apnea, and restless legs syndrome.
Environmental Factors Affecting Sleep at the End of Life

The environment in which an end-of-life patient lives can have a significant impact on their sleep quality. Factors such as noise, light, and temperature can all contribute to sleep disturbances. It is important to create a sleep-conducive environment that is quiet, dark, and cool.
Medical Interventions and Sleep at the End of Life

Medical interventions, such as medications, treatments, and procedures, can also affect sleep patterns at the end of life. Some medications can cause drowsiness or insomnia, while others can interfere with the body’s natural sleep-wake cycle. It is important to work with a healthcare professional to manage sleep disturbances caused by medical interventions.
Psychological and Emotional Factors Affecting Sleep at the End of Life
Psychological and emotional factors can also play a role in sleep disturbances at the end of life. Anxiety, depression, and grief can all make it difficult to fall asleep and stay asleep. It is important to address these psychological and emotional factors in order to improve sleep quality.
Sleep and Palliative Care

Sleep is an important aspect of palliative care. Palliative care providers can assess and manage sleep disturbances in order to improve the quality of life for end-of-life patients. This may involve using medications, non-pharmacological interventions, or a combination of both.
Case Studies of Sleep at the End of Life, Can you sleep in the end

Case studies of end-of-life patients with sleep disturbances can provide valuable insights into the causes and management of these disorders. These case studies can help healthcare professionals to develop more effective strategies for improving sleep quality in end-of-life patients.
Essential FAQs: Can You Sleep In The End
Why is sleep important at the end of life?
Sleep is essential for physical and emotional well-being. It helps the body heal, restores energy, and supports cognitive function. In the end stages of life, sleep can provide comfort, reduce pain, and improve overall quality of life.
What are some common sleep disorders in end-of-life patients?
Common sleep disorders in end-of-life patients include insomnia, sleep apnea, and restless legs syndrome. These disorders can be caused by various factors, including physical discomfort, medications, and psychological distress.
How can the environment affect sleep in end-of-life patients?
The environment can significantly impact sleep quality. Factors such as noise, light, and temperature can disrupt sleep patterns. Creating a calm and relaxing environment can promote better sleep.